IMPACT-breath Study Explores Non-invasive Diagnosis of Pseudomonas Aeruginosa Lung Infections in CF Patients
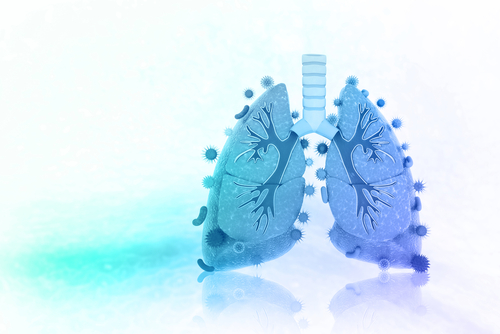
The diagnostic potential of breath analysis to detect serious lung infections in people with cystic fibrosis (CF) will be explored in a new clinical trial, which could lead to faster, more accurate diagnoses, and potentially improve the quality of life and prolong the life of these patients, researchers say.
The IMPACT-breath study will be led by Heather Bean, PhD, assistant professor at Arizona State University, who has been working to find new non-invasive diagnostic strategies to detect Pseudomonas aeruginosa infections.
Bean and collaborators will collect 288 breath samples from CF patients, 3 and older, from five hospitals across the U.S.
The chemicals present in each sample will be analyzed, and compared with the pattern of molecules produced by P. aeruginosa. This will allow the researchers to determine specific molecular profiles that can accurately distinguish which patients have lung infections caused by these specific bacteria or other strains.
IMPACT-breath is currently enrolling patients at Children’s Hospital Colorado, Phoenix Children’s Hospital, National Jewish Health, Dartmouth Hitchcock Medical Center, and Cincinnati Children’s Hospital Medical Center.
People with CF who are patients at one of these facilities can ask their physician for details. More information can also be found on the study’s webpage.
“These patients have seen the benefits of research during their lifetimes. They get new medicines that help them live longer,” Bean said in a news release. “They are so enthusiastic about participating in research studies and they’ll tell you it is the best part of their quarterly doctor’s visits. It’s been a real joy to directly interact with people who my work will benefit.”
IMPACT-breath is based on previous work by Bean and colleagues that showed that different strains of bacteria produce different volatile molecules. Detection of these molecules and how abundant they are can be used to build molecular profiles that are specific for each bacteria strain in both early and chronic infections.
First, the team identified these volatile molecules in cultures and in mouse samples. Then, they extended their findings to identify these chemicals in fluid samples taken from patient’s lungs.
“Typically, if we can catch the bacterium when it is colonized early in the patient, that leads to better outcomes. You have more options for antibiotics you can use,” Trenton Davis, research assistant in Bean’s lab, said. “If the patient has had that bacterium in their lungs for a while, that’s when you start seeing antibiotic resistance, and that really cuts back on the choices of therapy you have.”
Bean and her collaborators hope that the new IMPACT-breath study could lead to faster and more accurate diagnoses of lung infections in CF patients. This would have the potential to significantly improve the quality of life and increase the life span of these patients, the team believes.
The IMPACT-breath study is being supported by the Cystic Fibrosis Foundation and the National Institutes of Health.