Anxiety
Do Therapy Dogs Belong in Hospital Emergency Rooms?
Even a brief visit with a therapy dog can reduce anxiety in ER patients.
Posted May 16, 2019

My son Adam works in the trauma center in Mission Hospital in Asheville, North Carolina. With 100,000 admissions each year, the place is usually hopping. During a 12-hour shift, Adam will typically encounter some drug overdoses, a couple of heart attacks and broken bones, some car wreck victims, a few kids with a fever, and, occasionally, a stabbing or gunshot wound.
It’s a stressful workplace and once a week, a therapy dog named Brady and her handler pays a visit to the ER. The dog’s job is to help de-stress the doctors and nurses between patients. Adam tells me that a few of the ER staffers are not keen on having an animal in the emergency room. They find Brady a distraction, and one of the nurses mumbles that dogs spread germs. But the vast majority of the staff are happy to have Brady around. They are delighted to have a few minutes of mid-shift animal-assisted intervention now and then. But when I asked Adam if patients in the ER are ever allowed to interact with Brady, he said, “Nope, she is only there for the staff.”
Mission Hospital has an active therapy dog program for patients in other parts of the hospital. Why not for individuals waiting for treatment in emergency rooms? Wouldn’t they benefit from a bit of canine attention and affection? After all, many of them are stressed out. According to a new study published in the journal PLoS One, the answer is yes.
Therapy Animals in Hospitals
Research on the effectiveness of animal-assisted interventions in hospital settings has produced mixed results. Published studies have found that interactions with therapy dogs reduce the need for pain medication in surgery patients, decrease depression in individuals undergoing chemotherapy, and ameliorate anxiety in women hospitalized for high-risk pregnancies. Other studies, however, have been less encouraging. For example, investigators found that animal-assisted therapy had no effect on the psychological wellbeing of adults undergoing radiation treatments, that therapy dogs did not reduce pain in hospitalized children, or increase the well-being of kids undergoing chemotherapy. (See Media Coverage of Pet Therapy Often Gets It Wrong.) Indeed, one recent study reported that a stuffed dog was more effective than a real dog in reducing anxiety in adults who were awaiting surgery.
But until now, there has been no research on the impact of therapy dogs on patients in emergency rooms. The new study was conducted at the Sidney and Lois Eskenazi Hospital in Indianapolis by researchers from the Indiana University School of Medicine and the Center for the Human-Animal Bond at Purdue University. The team was led by Dr. Jeffery Kline, and their goal was to determine whether 15 minutes of interaction with a therapy dog would reduce anxiety in patients in the ER. What makes the study unique is that it is the first true randomized clinical trial of the impact of “pet therapy” in emergency room settings. Randomized control trials are considered the gold standard of medical research.
How to Study Therapy Dogs in Emergency Rooms
As reporter Karin Bruilliard pointed out in the Washington Post, much of the evidence that animal-assisted therapy works is flawed. The most common problems are insufficient numbers of subjects and a lack appropriate control groups. The Indiana University study was a methodological improvement over most of these studies. Patients in the hospital ER were asked if they would be interested in taking part in a therapy dog study. To participate, the patients had to be over 18 years old, awake, alert, and “not overly intoxicated.” In addition, they had to have been judged by an ER doc as experiencing “moderate or greater anxiety.” After excluding patients who did not meet the criteria, 80 individual participated in the research.
The patients were randomly placed in either the therapy dog group or a “usual care” control group. Patients in the usual care group were assigned to an individual room while they waited to see a doctor. Patients in the treatment group were introduced to a trained therapy dog and its handler just before they were assigned to an individual room. The dog/handler team remained in the room with the patient for 15 minutes. During this time, the patients interacted with the dog and talked to its handler.
The researchers expected that, compared to the usual care control group, patients who got to interact with the dog/handler teams would:
- have lower anxiety
- suffer less pain
- be less depressed, and
- have lower needs for opiate pain medications.
The patients rated their levels of anxiety, pain, and depression using variations of the scale shown below. On the scale, a 0 meant they were suffering no discomfort and 10 indicated they were
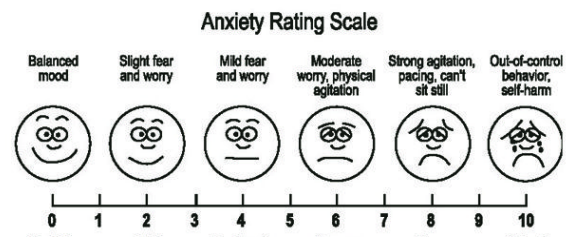
feeling extreme anxiety, pain, or depression. These are called “FACES Scales,” and they are widely used in medical settings. The scoring is reliable and the scales are easy to understand, even by people who are not literate.
All the patients completed the scales three times. The first was when they were initially assigned to an individual room in the ER (Baseline). The second was 30 minutes after the end of the dog visitation for the intervention group. (The control group completed the scale 30 minutes after beginning “usual care.”) Finally, the patients completed the scale once again (the Time 3 condition) just prior to discharge from the emergency room. This was typically an hour or two hours after the second administration of the scale. In addition, the dogs’ handlers took written field notes on the patient’s responses to the dogs.
Were the Therapy Dogs Effective?
The results were impressive. In the graph below, the median scores for the dog group patients are shown in green and the scores for the "usual care" patients are in red. At baseline, patients in both the dog group and the control group rated their anxiety as a 6 on the 10 point scale. (“Moderate worry, physical agitation”). But after just 15 minutes visiting with a therapy dog, the anxiety levels in the treatment group dropped to 2 (“Slight fear and worry”) while the control group scores did not budge. Even more impressive, the anxiety levels of patients in the dog group remained low for the duration of the ER visit. This typically lasted several hours. In contrast, anxiety levels of the usual care control group remained elevated for the duration of their time in the emergency room. While not as dramatic as the decreases in anxiety scores, the individuals in the dog group also showed substantially lower rates of pain and depression than the control group.
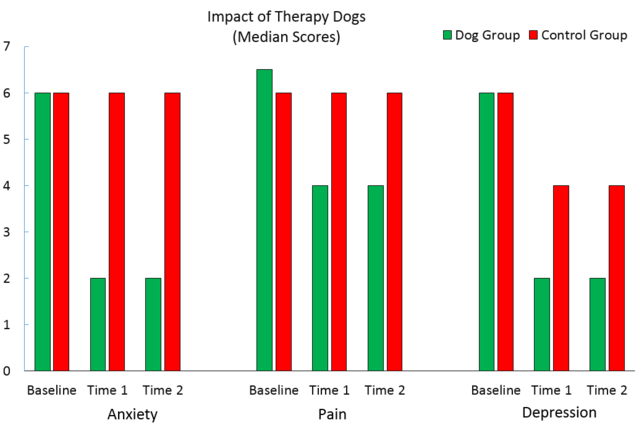
Further, only one of the 40 patients in the dog group needed opioid medication to reduce their pain compared to 7 of the 40 patients in the usual care control group. Similarly, only one of the dog group patients was given an anti-anxiety drug (by mouth), In contrast, seven patients in the control group required anti-anxiety meds (all of them by injection).
The field notes of the handlers also conveyed the impact the therapy dogs had on the patients. Here are three examples.
“The patient reached out to pet Cali and almost immediately changed from crying out loud to presenting a calm, inquisitive voice asking about Cali.”
“Within minutes, the patient’s demeanor had changed from being balled up on the stretcher, rocking back and forth, to on his hands and knees on the floor, playing with the dog.”
“With the family’s approval, patient and dog were happily relaxing together and it was evident to all those present (including the nurses) that this was the best thing that could have happened to that patient.”
Do Therapy Dogs Belong in Emergency Rooms?
This research is important and has applications in real-world settings. No study, however, is perfect. In this case, for example, the reductions in anxiety could have been caused by factors unrelated to the dogs. They could have been produced by, say, placebo or novelty effects. Or the conversations with the friendly handlers could have been the factor that relaxed the patients rather than the dogs. Finally, 81% of the subjects in the study were women, while half of the patients in the ER at the time were men. Whether animal-assisted therapy in this situation has different effects on men than women is unclear.
Despite these caveats, I’m impressed by the results of the study. I would, however, need additional evidence before I would recommend that hospitals start adding therapy dogs to their ER staffs. I would like to see the study replicated, ideally with more subjects with more men and with additional control groups. For example, one control group could eliminate the dog and simply have a friendly person talk to the patients for 15 minutes. When I ran this possibility by my wife Mary Jean, she did not buy it. She told me that talking to a person would not be nearly as effective as interacting with a therapy dog. “Dogs are special,” she said.
I’m inclined to agree.
References
Kline, J. A., Fisher, M. A., Pettit, K. L., Linville, C. T., & Beck, A. M. (2019). Controlled clinical trial of canine therapy versus usual care to reduce patient anxiety in the emergency department. PloS one, 14(1), e0209232.




