S. pseudopneumoniae Bacteria Can Cause Pulmonary Exacerbations in CF Patients, Study Finds
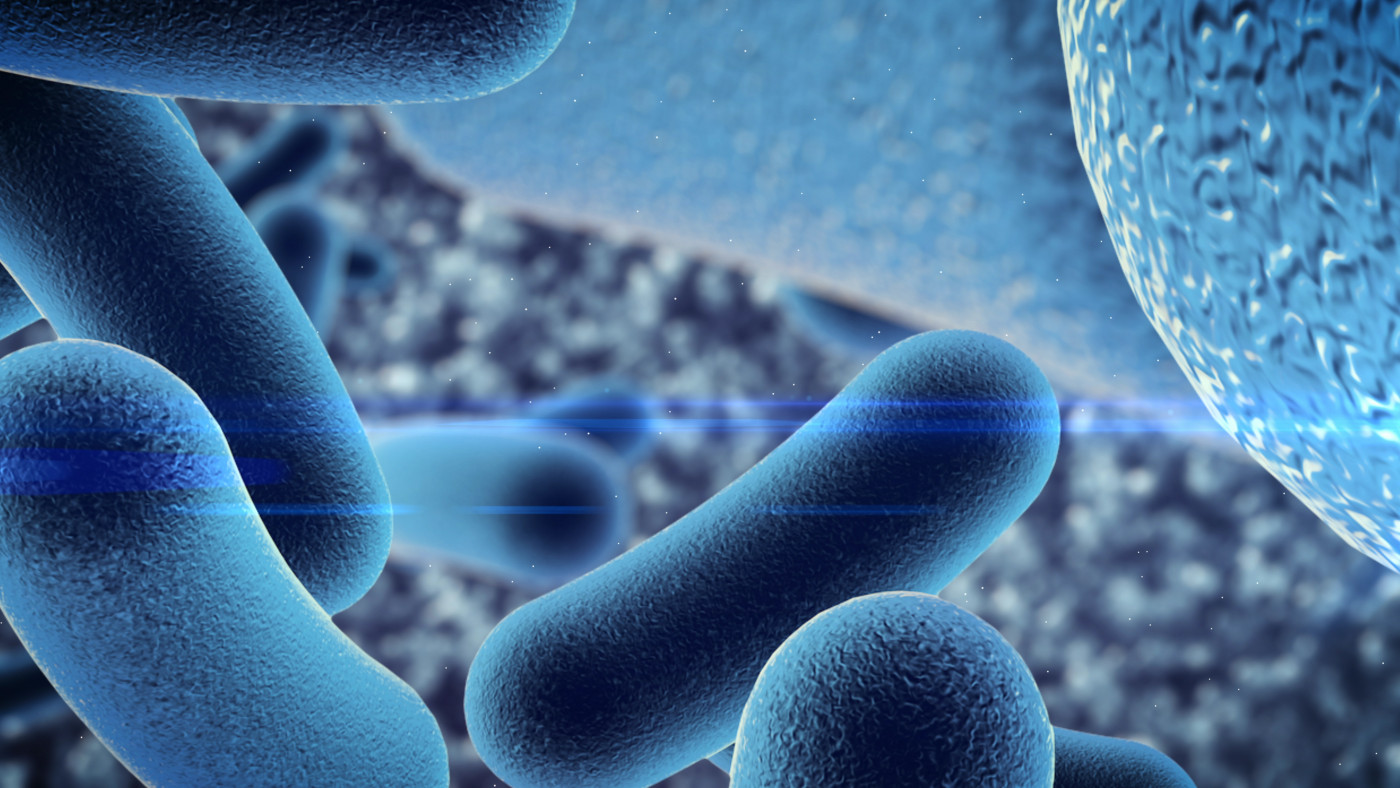
Streptococcus pseudopneumoniae should be included in the panel of opportunistic bacteria causing pulmonary exacerbations among those with cystic fibrosis (CF), according to a small French study.
The study, “Streptococcus pseudopneumoniae, an opportunistic pathogen in patients with cystic fibrosis,” was published in the Journal of Cystic Fibrosis.
S. pseudopneumoniae is a recently described species of bacteria that belongs to the “mitis group,” within the larger viridans group streptococci (VGS), a varied group of bacteria that colonize several tissues and organs, including the airways.
A previous study reported that Streptococcus bacteria is one of the most common types of bacteria found in the airways of children with CF during their first two years of life. Also, S. pseudopneumoniae has been classified as an opportunistic bacteria in people with chronic lung diseases, including chronic obstructive pulmonary disease.
However, little is known about the clinical impact of S. pseudopneumoniae on the health of those with CF.
To address that question, researchers in France reviewed clinical and microbiological data associated with S. pseudopneumoniae in a group of 20 CF patients, who had been routinely followed at the CF center at Montpellier University Hospital for a period of six years.
Through a combination of genetic tests, which included the detection of S. pseudopneumoniae through specific markers on patient respiratory tract samples, the team confirmed the presence of the bacteria in 13 of the 20 patients included in the study.
From these 13 patients (seven males and six females) whose samples tested positive for S. pseudopneumoniae, 11 (84.6%) were children younger than 10. The team hypothesized the higher incidence of S. pseudopneumoniae in children could be related to the high number of bacteria species found in children’s tonsils.
In 77% of the patients S. pseudopneumoniae was considered the dominant or co-dominant microbe. Six people also showed evidence of chronic colonization by Staphylococcus aureus, the most common cause of lung infections in CF patients during their first decade of life, and one patient by Pseudomonas aeruginosa.
Six patients (46%) had an episode of pulmonary exacerbation (symptom worsening) at the time of S. pseudopneumoniae isolation, which the team noted was comparable to the 35% rate of exacerbation associated with the presence of Streptococcus pneumoniae, another member of the “mitis group.”
“We showed that S. pseudopneumoniae … was associated with pulmonary exacerbation, either as the sole opportunistic pathogen or as part of a polymicrobial infectious process,” the researchers wrote.
Seven patients (54%) received an effective antimicrobial treatment against S. pseudopneumoniae, which consisted mainly of the antibiotic combination therapy co-amoxiclav.
Additional analyses showed that S. pseudopneumoniae was susceptible to several antibiotics, including amoxicillin, cefotaxime, pristinamycin, rifampin, vancomycin, and teicoplanin, and resistant or less susceptible to erythromycin, tetracycline, and penicillin.
Based on the results, the team suggested that “S. pseudopneumoniae should be considered as an additional opportunistic pathogen in CF,” they wrote.
“Our results warrant the need for additional studies to increase knowledge of the epidemiology and clinical significance of S. pseudopneumoniae in CF,” the researchers stated.
The team also noted that suitable laboratory tests should be developed and implemented in routine practice to prevent misidentification of bacteria species in patients’ samples, and the use of unsuitable antimicrobial treatments.
“Efforts towards accurate species identification are still required in routine practice,” the team emphasized.