Maximizing Clinical – Systems Aligns Nursing Practice with TIGER Initiatives
By Racquel Williamson, RN, BScN, MSN-INF
Abstract

Background
Safety in nursing reduces blame in the phrase, “to err is human” (Bates and Singh, 2018, p.1736). Adopting introspective analysis to expand on fixed patterns of feedback mitigates adverse events. This type of performance-based analysis in nursing reduces harm and enhanced knowledge for sustainable and effective solutions in maintaining quality nursing care. Maximizing clinical decision-supports prepares nurses to draw on analytics in interpreting nursing practice standards for patient safety. Globally, Patient Safety Organizations (PSO’s) have to minimize preventable harms and explore virtual platforms by using technology strategically to effectively engage nurses (Gallagher, Liske, and Widener, 2018). One way to mitigate medication and documentation structures analytically as an advanced practice nurse is to harness confluence analysis and accessibility factors. Currently, the burdens of medication errors to the public are multiplying. The cause of medication errors arises from poorly used health products and from poorly used systems. Evaluating systems and practices of care delivery with technology strengthens data, it strengthens processes, and it saves time evidenced by cost (World Health Organization, 2018a).
Objective
To integrate an e-booklet to show nurses how to proactively analyze and synthesize pharmacy audits collaboratively translates to augmented reciprocity in patient safety initiatives that are recommended by the World Health Organization (2018a).
The Purpose
Evaluating how nursing utilize medication and documentation practices while engaging with clinical decision-supports associates technology informatics guiding education reform (TIGER) initiatives in practice.
The Scope
When e-communication dash boards are maximized to debrief nurses on medication documentation safety, the outcome facilities tangible analysis in medication and documentation practices to meet health safety strategies
The Conjecture
If clinical decision-support dash boards are used efficiently to debrief nurses, will nurses cohesively interconnect medication and documentation practice standards? This integrated evaluation supports technology informatics guiding education reform (TIGER) initiatives to maximize technology and informatics into practice to augment patient safety (Healthcare Information and Management Systems Society (HIMSS), 2018).
Method
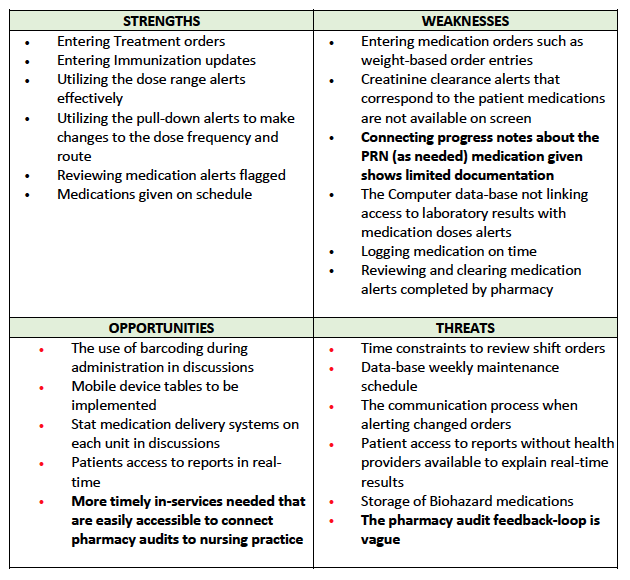
The evaluation utilized pharmacy audits along with reviewing the strength, opportunities, weakness, and threat (S.W.O.T) analysis of nurses to drive the gap analysis. This review was performed in an organization in Ontario, Canada that facilitated the implementation of a revised Clinical-Decision Support Database. The target audience were a mixed ratio of Registered Nurses and Registered Practical Nurses. The evaluation was conducted over a twelve-week time frame.
Extensive and randomized daily observation of the clinical data was reviewed anonymously to audit order sets: transcription, and documentation processes in real time. This information was aggregated. Then, an e-booklet was uploaded in the clinical communication dash board summarizing the evaluation. The e-booklet provided a comprehensive analysis of pharmacy audits while drawing on precedence and current nursing regulations. The analysis captured the S.W.O.T questionnaire survey, and inexpensively reviewed literature to facilitate pharmacy audits through a research perspective.
Results
This research facilitates better use of communication dash boards that maximizes accessible support systems to close the loop when translating patient safety data as an actionable quality improvement strategy. The effective use of clinical dash boards with nursing input is a consequential imperative when debriefing nurses on audits. Specifically, clinical audits in medication and documentation practice standards have to use similar principles by not only delivering feedback but including nursing analysis in the delivery of feedback data. Consolidating audits that maximize nursing inclusion factors along with maximizing clinical decision-supports strengthens knowledge translation, structures process analysis, and it is substantive in understanding paradigms of inquiry within disciplines to strengthen practice standards. Utilizing products and tools that are relevant and that are easily accessible fosters actionable sharing of information (World Health Organization, 2018a). The results show that nurses in this organization were at a ninety percent compliance relative to, the seventy percent compliance rate before the project was implemented. Real-time reports showed that within twenty-four hours nurses connected the Medication Administration Record (MAR) and used co-related progress notes ninety percent of the time with descriptive detailed assessment statements, after the e-booklet was embedded and read.
Keywords: Medication safety, clinical decision-supports, nursing documentation, nursing progress notes, analyze audits, proactively debriefs, nursing practice standards, (TIGER) initiatives.
An Analysis of Medication Management and Support Systems
Background
Patient Safety Organizations (PSO’s) have to minimize preventable harms with medication safety plans. Currently, the burdens of medication errors to the public are multiplying. An infamous 1984 Harvard Medical Practice Study (Brennan and Leape, 1991) was not the first study to investigate adverse drug events, but its findings were the impetus to standardize measures on this occurrence based on policy reform (World Health Organization, 2016).
The Canadian Medical Association and the Canadian Nurses Association’s principles on improving population health stipulated that more adaptable technologies for optimal management of care integrated delivery systems transforms governance. The Royal College of Physicians and Surgeons of Canada also released policy statements on integrated interdisciplinary collaboration as a key component in health organizations. More effective adaptation of health information technologies at point-of-care as a target plan, meets the needs of Canadians (Canadian Medical Association & Canadian Nurses Association, 2011).
Medication error incidents are linked to Prescriber error with inappropriate starting dose, dispensing errors, medication preparation errors, and monitoring systems errors. The cause of medication errors arises from poorly designed health products and can be amended by utilizing timely reciprocity systems. Adverse events reporting, and learning systems were developed by the World Alliance for Patient Safety in 2005 to help expand medication safety, facilitating changes at the local levels to mediate medication safety with triggering tools. Bringing awareness of gaps with nurses to light is strategic. Collaboration improves health culture, it strengthens the importance of reporting adverse events, and it advances communication on e-drug safety globally (World Health Organization, 2016).
Before automation, medication interpretation differed among nurses, pharmacists, and physicians. Today nurses specifically require prompt clinical decision support alerts that analyze and translate electronic medication audits to enhance the quality and safety of health care audits. This sharing of information closes the loop in medication safety. The proposed action was to implement an alert in the organizations communication dashboard to guide practice translation with electronic pharmacy audits. This adjunct review integrates timely evidence-informed communication with nursing practice and facilitates technology refinement in nursing informatics strategies (Canadian Nurses Association, 2006).
The case of A.M.C v. N.C in 2018 illustrated how to avoid negligence and reduce interpretation of evidence, if systems issues related to safe nursing care are investigated and utilized fully. Guay v. Wong in 2008 supported the premise of causation through inference of risk to show how trier of fact determines responsibilities in relation to vicarious liability. Understanding documentation practices and ensuring public safe was outlined in the College of Nurses of Ontario v. Lim case of 2012 in evidence tendered on how not meeting nursing’s medication standard of practice lead to the College on Nurses of Ontario revoking Lim’s certificate of registration (The Canadian Legal Information Institute, 2018).
The significance of this project was to reduce causal effects of medication management outlined by the World Health Organization (2016) by introducing structured analysis of medication management practices by nurses in organizations. The research question: If computer interfaces are maximized, will nurses maintain medication and documentation standards of practice? This integrated focus supports technology informatics guiding education reform (TIGER) initiatives to maximize technology and informatics as a change agent (Healthcare Information and Management Systems Society, 2018).
The Purpose
The focus of this project was to maintain nursing medication standards of practice through extrapolations, while utilizing automation in translational care. Decreasing the severity of medication incidence, shrinking the frequency of risks that contribute to errors, and increasing knowledge translation were key objectives. Constructive patient safety outcomes that integrate and embrace the use of technology dash boards progressed how information was received and perceived (Institute for Safe Medication Practice Canada, 2013).
The field of implementation science provided useful frameworks to draw from that emphasized that quality and consistency must be adaptive. Better understanding and maintaining dialogue within frameworks of laws to nurture public safety and expand collaborative exchange through coaching was a goal. Secondly, reviewing mechanisms that reduce barriers in facilitation and decision-supports, maintain fiduciary duties, and continue to collaboratively develop competencies in leadership drivers was critical in discovering the voice of the regulatory practice. Educational alerts have to contain inclusive exchanges to expand reciprocity in risk assessment (MHS Assessments, 2017).
Dr. Leslie Curry, Professor in Public Health Policy and Management at Yale University, focused on how qualitative research can be used to understand the depth of research such as implementing a new technology for context. Appreciating the potential of inclusive analysis generates actionable research concepts that transcend into sustainable health policy and management (Yale University, 2015).
Implementing an e-booklet that captures strengths, weakness, opportunities, and threats (S.W.O.T) of nurses with rigorous literature review is one patient safety health information technology (IT) strategy to engage innovation and collaboration into practice. The information gathered from this analysis can be used to forecast organizational predictive and retrospective analytics. Advanced practice nurses have to develop needs assessments, translate evidence into practice, and develop and evaluate the learning management systems so, that meaningful translational information continues to be timely, responsible, and collaborative (Sipes, 2015).
Focus of Inquiry
Information exchange related to e-medication management audits have to be presented in conjunction with nursing analysis, so that members are better prepared to meet medication standards of practice that are outlined by the College of Nurses of Ontario (College of Nurses of Ontario, 2018). This collaborative movement will lead to positive gains to increase understanding, to share cost, to enhance quality programs, and decrease mitigated risk. Interoperability measures that are value-based advances safety in caring for populations (World Health Organization, 2010).
Evidence accumulated from Statistics Canada has shown that medication errors are aggregated by clinical electronic records sharing. Nurses are at time focused on when the research community investigates medication-related errors. Nurses clarify ambiguous orders and nurses have the knowledge to question orders. The broader context research shows that the complex clinical environments, rather than the individual professional contributes to risk and negligence. The National Survey of the Work and Health of Nurses (Wilkins & Shields, 2005) collected data responses and offered an opportunity to study medication errors based on the Donabedian’s structure-processes. Outcome frameworks in this area found that analyzing actual performance with desired performances with accessible technology reduced errors. Analytical logistic regression analysis suggested that confidence intervals on medication error analysis shows that medication errors occur in phases such as prescribing, dispensing, administration, and monitoring. Integrating system development life cycle applications to understand and guide methods in this practice gap advances strategies in safe-medication processes (Institute of Safe Medication Practices Canada, 2018).
Needs Assessment / Gap Analysis
Current Situation: Currently, there are medication management gaps within the electronic health system. Nurses are aware of medication management discrepancies through pharmacy audits, but that data is not synthesized through a collaborative approach to maintain medication and documentation standards of practice.
Gap: There needs to be information designs that analyzes medication and documentation practices collaboratively to debrief nurses on nursing practice standards.
Goal: The goal was to upload an analysis of e- medication management data in the organization communication dashboard. The secondary goal was to show nurses how to synthesis pharmacy feedback proactively to build capacities in patient safety.
S.W.O.T Findings
Review of Literature
Quantitative research has been done which proposed that analyzing medication safety has to have an inter-professional approach. This enables nurses and the pharmacy team to learn from experience. This is a key inter-professional strategy to increase comprehensive documentation of drug management (Bell, Granas, Enmarker, Omol, and Steinbekk, 2017).
Further research inquiries have shown that knowledge translation strategies enhance health professional, organizational, financial, and regulatory decision-making. Evidence-informed decision-making with nurse inclusion closes the gap between knowledge and actions (Yost, Thompson, Ganann, aloweni, Newman, McKibbon, Dobbins, and Ciliska, 2014).
Medication safety prior to the adoption of electronic health records added redundancies that cost money, slowed innovation, and hindered communication mediums. The complexity of medication management must be paralleled with assessment, evaluation, policy, and technology to provide substantive recommendations in medication and documentation cohort analysis. Auto-populated electronic MARs or automated nursing alerts improve system design and processes to integrate substantiate de-briefing (Pascale, Wetterneck, Cartmill, Blosky, and Brown, 2014).
Honorable Beverley McLachlin informed us that listening, making efforts in cheering for value-based conversations, and encouraging collegiality propels advancements in the partisan of the constitution. Policy judgements with collaboration provides good results and is a sound value judgement. Interactions cannot be silent. It has to be weathered, it should be questioned, and compared to due processes as it related to sufficient detail (CBC News: The National, 2017).
Working with stakeholders to amend medication safety with sustainable analytics strategies is a global initiative to strengthen health excellence. Conducting a series of allegations with discovery, that introduces amendments is upheld by law. Forms of case analysis is historical, contextual, and constraining, but introduces optimization that empowers authorities (World Health Organization, 2016).
Practicum Methodology / Procedures
- Step 1: Perform a literature review to support the mini gap analysis findings by August 27, 2018
- Step 2: Conduct a gap analysis by August 27, 2018
- Step 3: Conduct a SWOT analysis of peer feedback to drive the e-booklet clinical quality assurance and safety objectives in electronic health record medication ordering by August 27, 2018.
- Step 4: Implement an e- booklet with content analysis by the end of October 2018.
- Step 5: Upload the e-booklet to the clinical dashboard communication message tab for one month or for as long as the organization authorizes by the second last week of practicum.
- Step 6: Prepare an end of project feedback survey to evaluate the hypothesis: if e-booklets are designed into an organization intranet to collaborate with pharmacy audits, health organizations will be better prepared to support safe e-medication management by October 2018.
Practicum Project Resources
Direct Resources
Direct resources included the health management team, the organizations’ pharmacy audits, the nursing team, my practicum mentor, the University of Phoenix (UOP) practicum professor, and the writer.
Indirect Resources
Indirect resources included the pharmacy audits, literature review journals, the University of Phoenix (UOP) e-book resources, the UOP library database, the World Health Organization (2016, 2018a) recommendations, the College of Nurses of Ontario guidelines (2018), the Registered Nurses’ Association of Ontario recommendations (2018), Google, Google scholar, and citations from the Canadian Legal Institute (2018).
Applicable Compliance
There are several legislated guidelines that all health professionals, including nures must follow. For instance, in the United States, nurses have to be compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA) that protects health information, and the Health Information Technology for Economic, and Clinical Health Act of 2009 Title X111 (HI-TECH Act). In Canada, nurses must follow applicable federal and provincial guidelines, such as the need for Ontario nurses to comply with the Personal Health Information Protection Act of 2004 section A. The federal Personal Information Protection and Electronic Documentation Act of 2000 (PIPEDA) and the Digital Privacy Act of 2015 stipulate applicable laws that must be adhered to by all Canadian nurses when maintaining public safety (Anonymous Health Organization, 2018).
To handle applicable compliance the project adhered to the above laws since the writer read and understood the legalities on digital transactions and governance with UOP guided legal authorization. The writer used evidence-based best practices for reducing legal and security compliance risk by monitoring the uploaded project according to the signed UOP agreement.
Regulatory Requirements
When reviewing medication safety deductively, a global reduction of medication harm by fifty percent is recommended (The World Organization, 2016). Medication reconciliation across transitions of care through Safer Healthcare Now is performed by nurses to improves medication reconciliation (The Institute of Safe Medication Practices Canada, 2018).
Nurses meet regulatory medication standards when authority, compliance, safety, and a decision tree are adhered to for public safety (College of Nurses of Ontario, 2018). Nurses in an organization have to be 100 percent compliant with medication management policies supported by pharmacy audits (Anonymous Research Organization, 2018).
Compliance will be successful when as needed (PRN) medication order entries have at least ninety percent compliance with progress notes that are corroborated with real-time pharmacy audits. Nursing connecting documentation entries with medication errors will decline quarterly (Registered Nurses’ Association of Ontario, 2013).
The writer outlined College of Nurses of Ontario medication standard requirements (2018) and identified and remediated vulnerabilities based on management suggestions. The management team were updated weekly on the progress of the project to expand utilized focused exchange processes. Making sense of data comes with collaboration. This type of exchange called on understanding the buying-in phase as the intended beneficiary related to the preponderance of evidence (Quinn, 2012).
The writer also reviewed and analyzed medication-reconciliation documents, physician order entries, the Medication Administration Record, and the progress notes processes over the practicum observation time-frame and introduced the e-booklet to facilitate structured guidance in showing nurses tangible evidenced-informed analysis of this medication safety gap.
Project Implementation Plan
Design Objectives
- To have the project run on existing networks used by the organization.
- The project will run on a SQL database
- The implementation will be compatible with Java programming language.
- Prioritizing requirements:
- The e-booklet must be uploaded by the end of October 2018.
- The project should incorporate the gap analysis, literature review, and regulatory information.
- The project design may contain graphics to add to the visual appearance and the cache principles.
- The project design would be more effective if management agrees to embed this process with future communication too nurses.
- Performance testing was done prior to October 2018 to ensure the e-book application was viable without setting of system alerts. The performance testing was done by the end of September 2018. This testing assessed the response time, reliability, usage, and scalability of the project tool by showing no pop-up alerts.
Cost Benefit Analysis
Developing a sustainable cost benefit project document measures performance against constraints. This document outlines time, cost, quality, risk, and scope of the project that are aligned to reduce mitigated risk. The cost benefit analysis outlines the Plan, Do, Check, Act (PDCA) process to track project tasks and deliverables (Sipes, 2015). The actual cost of developing this project is thirteen dollars and fifty cents, based on the calculations in the cost benefit document.
Plan
To design an e-booklet to upload in the intranet communication dashboard to analyze nursing e-medication management. This design collaborates with pharmacy audits and nursing actions when pharmacy audits are reported.
Do
This plan was implemented during the practicum time frame influenced by the SWOT analysis, determined by the gap analysis, gauged by the literature review, and measured by regulatory requirements.
Check
The e-booklet implementation was measured by the end of project survey responses in November 2018. Management were updated weekly on the progress of the project. Performance testing was done in September 2018 and the e-booklet was implemented in November 2018.
Act
The implementation design collaborated with the pharmacy audits to maintain nursing medication practice standards mandated by the College of Nurses of Ontario (CNO, 2018) and supported by the World Health Organization (2016) recommendations.
S.M.A.R.T Objectives
S =The e-booklet will be implemented in the communication dashboard for nurses to review, reflect, and improve on e-medication management synthesis.
M = The measure is effective when nurses in the organization review the e-booklet, when nurses verbalize positive feedback with the end-of-survey form, and when the next pharmacy audit shows reduced e-management concerns.
A = This implementation design will be achievable within the project time allotted by the practicum agreement time frame. The estimated budget to complete the project design is ten to fifteen dollars. The resources used will be the management team, the SWOT survey, and the pharmacy audit indicators.
R = The objectives comply with the organization’s mission to improve e-medication management with the EHR for patient safety.
T = The due dates for each task are assigned. Please refer to the project scope.
Risk Management Plan
The integration of quality management systems can bring organizations incalculable advantages. Risk management agendas are aimed at preventing risk or harm thus providing quality care (Costa, Meirelles-Schlindwein, and Erdmann, 2013). This risk plan minimizes the practice gap to show that when technology is utilized and when technology is easily accessible, nurses will continue to adhere to medication practice standards. This phase of this project draws on theoretical data and ethics to frame nurses accounts of computer systems that are linked to strengths, weakness, opportunities, and threats with medication management. The aim in this risk management plan is to identify potential sources of risk. The risk plan chart to proceed will help decide what, if any issues may impact the project, and outline solutions to decrease the degree of probability. (click to view risk plan chart)
Methods
This paper provides an extensive literature review on a specific strategy to augment TIGER initiatives in nursing practice. The evaluation utilized pharmacy audits along with reviewing the strength, opportunities, weakness, and threat (S.W.O.T) analysis of nurses to drive the gap analysis. This review was performed in an organization in Ontario, Canada that facilitated the implementation of a revised Clinical-Decision Support Database. The target audience were a mixed ratio of Registered Nurses and Registered Practical Nurses. The evaluation was conducted over a twelve-week time frame.
Extensive and randomized daily observation of the clinical data was reviewed anonymously to audit order sets: transcription, and documentation processes in real time. This information was aggregated. Then, an e-booklet was uploaded in the clinical communication dash board summarizing the evaluation. The e-booklet provided a comprehensive analysis of pharmacy audits while drawing on precedence and current nursing regulations. The analysis captured the S.W.O.T questionnaire survey, and inexpensively reviewed literature to facilitate pharmacy audits through a research perspective. Some nurses were observed to demonstrate a dampened behavioral response when pharmacy audits were mentioned. The needs assessment found that this gap in nursing practice hampered nursing excellence in practice. The e-booklet described the process used to guide nursing standard expectations similar to a second order process that predicts performances.
Preparing a comprehensive analysis in the database communication dash board, rather than setting up a timed teaming or imputing real-time audit statistics with descriptive words, provided nurses with a substantive break-down that shifted nursing medication and documentation practices. After the e-booklet implementation the organization yielded a ninety percent compliance rate to medication and documentation nursing standards. The transfer of accountability was evident in twenty-four hours, once the e-booklet prompt was read by nurses. Observational and compliance evidence revealed that the nursing compliance ratio with medication quality indicators were maintained at a steady curve and continued beyond the evaluation time. The evaluation was set to delete after three months. Measuring the implementation deletion timeframe was aligned with quarterly quality improvement sustainability tools philosophy that focused on measuring outcomes and process quarterly when scaling algorithms (Ideas Ontario, 2014).
Metrics for Success
The metrics for success were demonstrated by: maintaining the cost schedule, showing that the project implementation meets security compliance; demonstrating that the project uploaded without error alerts; reviewing if pharmacy audit reports improved in the next quarter analysis, the uploading of the e-booklet into the organizational data-base, and lastly, were demonstrated with improved MAR and progress notes by nurses in the organization. This engaged collated feedback that reinforces and moderated the inquiry. When re-evaluating the research, applying theoretical integrity that considers sub-structs responses to conclusions is important. Setting up indicators with reflection and response options related to the needs analysis to meet the project goals. Future research must broaden staff expectations through a shared medium to improve performance triggers (Rapley, Girling, Mair, Murray, Treweek, McColl, Steen, May, & Finch, 2018)
Program Adaptation
Initially, the project adapted to the clinical area when management agreed to its implementation. As well, the project adapted by minimizing risks by sticking to the schedule and budget. and detecting problems early by reviewing real time audits five out or seven days a week, and keeping all people involved utilizing full disclosure based on the University of Phoenix signed Agreement Contract between myself and the organization.
Results
There was a ninety percent amendment in practice that linked medication administration practices to detailed progress notes evidenced by pharmacy audits and daily real time observational methodology within the practicum time frame. Once the e-booklet debriefing tool was uploaded nursing connected medication and documentation standards in the clinical system rose from 70 to 90 percent compliance. Management revealed that there were not only more detailed reports to review that met Nursing Standard of Practice, but specifically, that nursing practice behaviour shifted in asking detained questions when interacting with pharmacy, and that verbal, non-verbal, and written communication to pharmacy were timely, transparent, and accountable (Anonymous Health Organization, 2018).
When information systems are maximized the facilitation of information exchange competencies augments patient safety to meet TIGER initiatives and ultimately meets Ontario nursing practice standards. On a macro level, global initiatives that expand and prioritize collaborative health technologies enriches health systems. This learning domain interfaces professional leadership with research, it advances roles and responsibilities in containing cost, and it allocates reflection in health expenditures to the health environment as it relates to big-data streaming analytics (World Health Organization, 2010).
Appropriately documented health systems review with aggregation of trends relates to cohesive innovations in the delivery of care quality so, that time, skills, knowledge translation, and processes in the workforce identifies and mitigates practice-gaps collaboratively. This form of data adaptation is essential in facilitating pragmatic, sharing of information in health domains globally. Collecting statistics, designing aligned systems, and reporting of information to Health Canada on the management and prevention of medication safety is essential when analyzing health policy indicators (Canadian Center for Policy Alternative, 2011).
Evaluation of Program Success
The project was deemed successful once it was uploaded into the organizations’ intranet. It was also deemed successful when the design objectives were met, management and the nursing team verbalized and demonstrated changes in practice to maintain CNO practice standards, and the University of Phoenix MSN-INF core objectives were met by the writer receiving an MSN-INF designation.
Implications
The reduction of causal effects in medication safety as outlined by the World Health Organization by introducing structured analytics collaboratively in clinical decision-supports prioritized safety efforts and closes the loop in medication safety to meet TIGER initiatives that advance Informatics practices in health safety (World Health Organization, 2016).
Conclusion
“The ultimate purpose of metrics and dashboards is not to provide more information but to provide the right information to the right persons at the right time…Project management is an attempt to improve efficiency and effectiveness in the use of resources” (Kerzner, 2017, p. ix). Implementation plans are fluid methodologies capable of interfacing with the business process related to the Triple Aim to improve patient experience, to improve health population, and to reduce per capita cost (Institute for Health Improvement, 2018). This project demonstrates how the e-booklet methodology is a realistic intervention and is easily accessible, which helps nurses continue to adhere to College of Nurses of Ontario (2018) practice standards through the power of inclusive data set analytics.
References
Anonymous Health Organization. . (2018). Authorized for Research Evaluation. Ontario: Canada.
Bates., D.W., and Singh, H. (2018). Two decades since To Err is Human: an assessment of progress and priorities in patient safety. Agency of Healthcare Research and Quality. 37,1736-1743. Retrieved from http://www.psnet.ahrq.gov.
Bell, H. T., Granas, A. G., Enmarker, I., Omil, R., and Steinsbekk, A. (2017). Nurses’ and pharmacists’ learning experiences from participating in interprofessional medication review for elderly in primary health care – a quantitative study. BMC Family Practice. 18,2-9.
Brennan, T. A., & Leape, L. L. (1991). Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study. Perspectives In Healthcare Risk Management, 11(2), 2–8.
Canadian Center for Policy Alternatives. (2011). Health Care.Retrieved from http://www.policyalternatives.ca.
Canadian Medical Association & Canadian Nurses Association. (2011). Health Care Transformation in Canada. Retrieved from https://cna-aiic.ca/~/media/cna/files/en/guiding_principles_hc_e.pdf
Canadian Nurses Association. (2006). E-nursing strategy for Canada. Retrieved from https://www.cna-aiic.ca/~/media/cna/page-content/pdf-en/e-nursing-strategy-for- canada.pdf?la=en
CBC News: The National. (2017, Dec. 18).Beverley McLachlin reflects on supreme court career, dispute with PM Harper.[Video file]. Retrieved from https://youtu.be/VLEogRtquaQ
College of Nurses of Ontario. (2018). Medication.Retrieved from http://www.cno.org.
Costa, V. T., Meirelles-Schlindwein, B. H., and Erdmann, A. L. (2013). Best practice of nurse managers in risk management. Revista Latino-Americana Enfermagem. 21(5), 1165-1171.
Gallagher, M.R., Liske, D.C., and Widener, J. (2018). Digital Disruption: Transforming Collaboration and Engaging Nursing Leaders. Retrieved from http://www.stti.confex.com.
Healthcare Information and Management Systems Society (HIMSS). (2018). TIGER Initiative for Technology and Health Informatics Education. Retrieved from https://www.himss.org/what-we-do/Initiatives/tiger
Ideas Ontario. (2014). Share Ideas: Health Care Quality Improvement (QI) Project Repository. Retrieved from http://www.quorum.hqontario.ca.
Institute for Healthcare Improvement. (2018). IHI Triple Aim Initiative. Retrieved from http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx
Institute of Safe Medication Practices Canada. (2018). Ontario Critical Incident Learning. Retrieved from http://www.ismp-canada.org.
Kerzner, H. (2017). Project Management: A Systems Approach to Planning, Scheduling, and Controlling.(12thedition). Hoboken: New Jersey: Wiley.
MHS Assessments. (2018). Online Assessment Center. Retrieved from https://mhs.com/clinical-assessments/online-assessment-center/
Mitchell, L. (2015). Does Medical Education need a Revolution?University of Toronto Medicine. Retrieved from https://medicine.utoronto.ca/news/does-medical-education-need-revolution
Pascale, C., Wetterneck, T. B., Cartmill, R., Blosky, M., and Brown, R. (2014). Characterizing the complexity of medication safety using human factors approach: an observational study in two intensive care units. BMJ Quality and Safety. 23(1), 56.
Quinn, M.P. (2012). A utilization approach to contribution analysis. Evaluation. 18(3), 364-377.
Sipes, C. (2015). Chapter 5: Implementation/execution – Phase 3. Project Management for the Advanced Practice Nurse, 93-114.
Rapley, T., Girling, M., Mair, F.S., Murray, E., Treweek, S., McColl, E., Steen, I.N., May, C.R., and Finch, T.L. (2018). Improving the normalization of complex interventions: part 1 – development of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Medical Research Methodology. 18(1), 1-17.
Registered Nurses’ Association of Ontario. (2018). Nursing Best Practice Guidelines. Retrieved from https://rnao.ca/bpg
Registered Nurses Association of Ontario. (2013). Assessment and management of pain.Retrieved from https://rnao.ca/sites/rnao-ca/files/AssessAndManagementOfPain_15_WEB-_FINAL_DEC_2.pdf
The Canadian Legal Information Institute. (2018). Retrieved from http://www.canlii.org.
Watt, A. (2016, March 4). Medication Safety at Transitions of Care. Institute for Safe Medication Practices Canada. Retrieved from https://www.ismp-canada.org/download/presentations/PPLNetworkmarch42016.pdf
Wilkins, K. & Shields, M. (2005).The National Survey of the Work and Health of Nurses.Statistics Canada. Retrieved from https://www150.statcan.gc.ca/n1/pub/82-003-x/2008002/article/10565-eng.htm
World Health Organization. (2018a). Patient Safety. Retrieved from https://www.who.int/patientsafety/en/
World Health Organization. (2018b). Oral Health. Retrieved from http://www.who.int.
World Health Organization. (2016). Medication Errors. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/252274/9789241511643-eng.pdf;jsessionid=724147C214BA22806CE11A3957B31BCB?sequence=1
World Health Organization. (2010). Frameworks for Action on Interprofessional Education & Collaborative Practice. Geneva: WHO. Retrieved from https://www.who.int/hrh/resources/framework_action/en/
Yale University. (2015). Fundamental of Qualitative Research: Models 1-6. Retrieved from http://www.publicheatlh.yale.edu.
Yale University. (2019). Lecture 18 – Imperfect Information: Sets and Sub-Game Perfection. Retrieved from http://ocy.yale.edu.
Yost, J., Thompson, D., Ganann, R., Aloweni, F., Newman, K., McKibbon, A., Dobbins, M., and Ciliska, D. (2014). Knowledge Translation Strategies for Enhancing Nurses’ Evidence-Informed Decision-Making: A Scoping Review. World-views on Evidence-Based Nursing, 11(3), 156-167.






