How a continence nurse specialist overcame barriers to introduce a brand new continence service to improve patient care and experience across a trust that provides acute and community services to a population of nearly one million people
Abstract
In 2019, East Suffolk and North Essex NHS Foundation Trust launched a quality improvement project to review how it promoted continence. This led to the introduction of a new continence service with a revised continence assessment, training and education plan, which aims to raise awareness of the importance and impact that good continence care has on patients and their outcomes.
Citation: Woollerton T (2023) Don’t just grab a pad: introducing an effective continence service. Nursing Times [online]; 119: 4.
Author: Teresa Woollerton is continence nurse specialist, East Suffolk and North Essex NHS Foundation Trust.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
East Suffolk and North Essex NHS Foundation Trust (ESNEFT) began investigating the possibility of introducing a continence service for adults in 2019. At the time, one of the two acute hospitals run by the trust had no such service, while the other offered a continence assessment – which was rarely used – and provided very little guidance on effective ongoing continence care. In addition, anecdotal evidence from patients, relatives and staff suggested that patients – often those who were older people – were sometimes given continence pads without any discussion, while others were put in pads because no-one was available to take them to the toilet. As an example, one relative said her father had been told he didn’t need urine bottles overnight as he was wearing a pad.
This approach was not limited to ESNEFT; interviews with nurses, medics and other health professionals carried out by Percival et al (2021) showed that continence care was often a low priority in acute trusts, with very little training provided. As a result, continence issues were regularly missed and other tasks were often perceived as more important by staff, who were under time pressure. Patients would even accept wearing pads, instead of asking for help to get to the bathroom.
Unfortunately, some patients reported that they were continent before their admission to hospital, but incontinent by the time they were discharged home. This was highlighted in a recent study by Featherstone et al (2022), which found that patients with dementia were expected to use continence pads, whether or not they were incontinent. This led to these patients becoming incontinent and losing some of their independence in a trend referred to by the authors as “pad culture”.
As well as having a negative affect on patients and their experience of receiving care, this approach is also costly, with the NHS spending an estimated £80m a year on continence products (NHS England, 2018). In addition, statistics show that patients who are incontinent are 26% more likely to fall and 34% more likely to have a fracture (NHS England, 2018). Incontinence is also a significant factor in incontinence-associated dermatitis (IAD) (Flanagan, 2020).
A study carried out by Moon et al (2021) concluded that the need to urgently and frequently pass urine, combined with poor mobility, was likely to contribute to increased falls among this patient group. In addition, Voegeli (2017) stated that prolonged exposure to urine and faeces could lead to IAD. He concluded that nursing staff often confuse IAD with pressure sores, and that carrying out an assessment to help identify incontinence would mean that the right care could be put in place to avoid IAD.
Piloting a continence service
At ESNEFT, which includes two acute and five community hospitals, there was often no nursing rationale or assessment for the continence products used. Inappropriate use of continence pads was also a factor in deconditioning patients and costly for the trust. As detailed earlier, the evidence also suggested this was happening nationally, with continence care often overlooked (Voegeli, 2017).
To address this at ESNEFT, a continence project board was set up by a:
- Senior matron in one of the acute hospitals;
- Community continence lead;
- Head of procurement.
After reviewing referrals from our hospitals to community teams and anecdotal evidence from patients, they identified a need to appoint a continence nurse specialist who would:
- Promote continence awareness among staff and patients, and introduce an education programme;
- Reduce the number of falls and moisture damage associated with poor continence care;
- Reduce the deconditioning of patients through good continence care;
- Stop the overuse of ‘all-in-one’ pads, which were most commonly used across the trust, but not recommended for widespread use by the Association for Continence Advice (ACA) (2021) – instead, the ACA advises that pads and pants should be used in the majority of cases;
- Produce a continence assessment and care plan to be used consistently across the entire trust to promote good continence care;
- Liaise with the community continence teams to ensure continuity of care from hospital to home, starting with basic continence conservative treatment during the patient’s admission.
I came into post in 2021 and began a quality improvement (QI) project, initially as a three-month pilot on four wards (three care of older people wards and one orthopaedic ward), where staff had voluntarily expressed an interest in improving continence care. I liaised with the community continence teams and used guidance from the National Institute for Health and Care Excellence (NICE), NHS England and the ACA, which stated:
- Patients with urgency and frequency of urine should be offered six weeks’ bladder training, which begins in hospital before discharge and continues in the community (NICE, 2019);
- All patients should have their continence assessed and treatment commenced before containment products, such as pads, are introduced (ACA and RCN, 2021).
I then produced clear guidelines and a user-friendly continence assessment and care plan (Fig 1). These documents were patient centred, promoted continence and encouraged staff to start continence-conservative treatment – such as simple lifestyle changes to diet – for patients who were on the wards.

As there was previously no continence service at Colchester Hospital, the baseline for assessments, continence care and the rationale for using products was set at 0%, and the target set at 50%. For patients, this meant:
- Assessing them for any continence issues;
- Finding the best treatment and products to either manage or improve their continence and, in some cases, help them to become continent again.
This would, in turn, reduce their risk of IAD, falls and deconditioning.
As staff were not used to assessing patients for continence care, I also developed an education programme devised by the ACA (2021). This was available in a variety of formats, such as:
- In-person and virtual presentations;
- e-learning;
- Face-to-face sessions;
- Working one-to-one with individuals.
I also made sure I was available to work with staff and patients on the initial four wards, and give help and advice on a regular basis for the duration of the pilot. The training was designed to cover basic continence care and conservative treatment, and was in line with the basic assessment of incontinence, for staff, as outlined in the United Kingdom Continence Society’s (2015) Minimum Standards for Continence Care in the United Kingdom.
Although the training was designed to show colleagues how to assess a patient’s continence and basic conservative treatment, it also prompted lots of discussion around the attitudes of both staff and patients to incontinence. For example, some staff previously thought the most-effective way to manage the condition was to give patients the most-absorbent pad available, while others were unaware of the different types of incontinence – even common types, such as urgency and frequency, or stress incontinence. This meant that they were not familiar with basic conservative treatment, such as fluid modification and bladder training. In addition, a lot of patients were surprised to learn that there were steps they could take to improve their continence; they often thought it was an inevitable consequence of ageing. This highlighted that patient education was also an important part of continence care.
An audit based on the Guidance for the Provision of Absorbent Pads for Adult Incontinence: A Consensus Document, published by the ACA and Royal College of Nursing (RCN) in 2021, was carried out at the end of the three-month pilot. It showed the improvement in continence care had far exceeded our original target (Table 1).
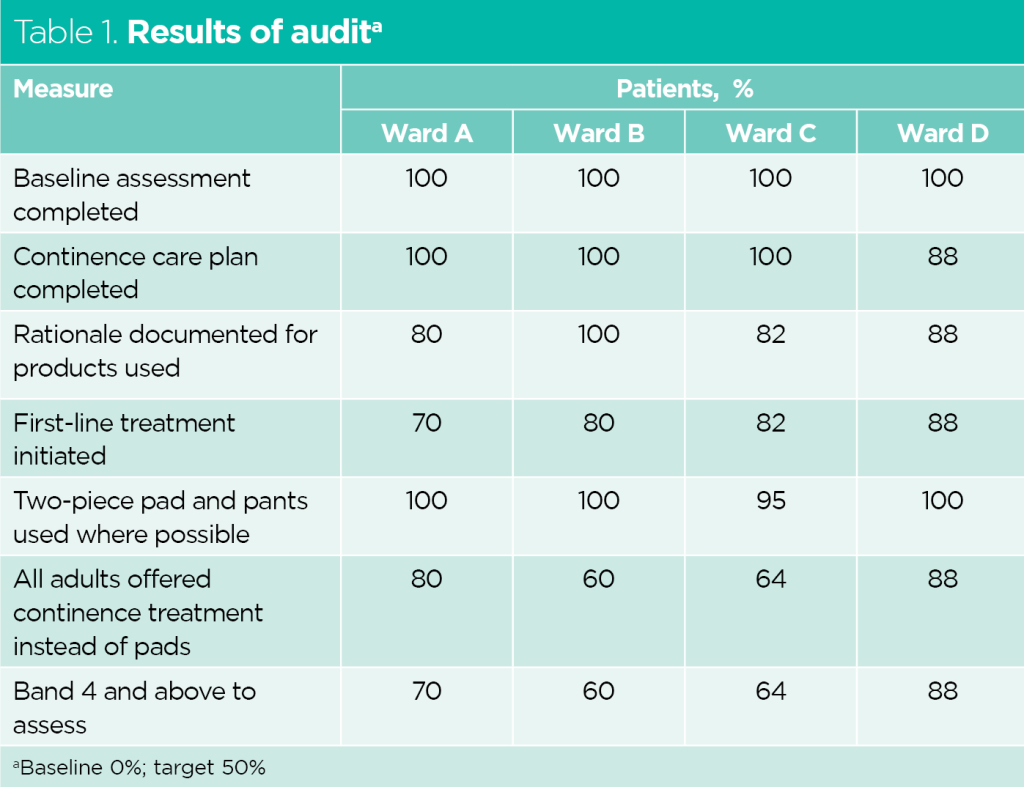
In addition to providing good continence care for patients, the pilot resulted in a cost saving of £835.78, compared with the same period in 2020. This was mainly due to using fewer pads on the four wards between April and June 2021; over a 12-month period, this would amount to a saving of £3,343 for these four wards alone.
Learning from the pilot
The pilot demonstrated that, to have effective change in continence care, staff need:
- Regular training and support;
- The right tools, including an effective assessment and care plan;
- The correct products to suit the patient’s needs;
- Support with using these products effectively and appropriately.
The pilot also showed us that good working relationships with other organisations were important for the success of the project. Continence nurses from outside of ESNEFT were happy to share their experiences and examples of best practice to help us shape our new service. In addition, incontinence-pad companies:
- Provided useful training on how to use products effectively;
- Explained how each product worked;
- Raised awareness about the fact that using the largest and most absorbent for every patient was not necessarily the right approach.
As the figures from our audit show, the initiative also had the potential to deliver substantial cost savings for the trust. We hope it will reduce falls and incontinence-associated dermatitis in the future.
Sustainability and spread
Following the success of the pilot project, the fledgling continence service was rolled out across the whole trust, including all the remaining wards at Colchester Hospital, as well as across Ipswich Hospital and ESNEFT’s five community hospitals. As the trust employs more than 10,000 staff and has nearly 50 wards in its acute units alone, this was a huge task.
The first step was to gain approval from our patient safety group on the continence assessment and care plan, which was then adopted as a trust-wide document. I also worked closely with IT and the education department to find different ways of offering continence training.
As the initiative was rolled out during the Covid-19 pandemic, Microsoft Teams and online training became essential tools for reaching a wide audience, which started with staff and then included patients. This also allowed us to easily invite other organisations, such as continence companies, to take part in the training to share learning and increase participants’ knowledge of the importance of good continence care.
The Covid-19 pandemic left many teams facing staff shortages and under increased pressures, so rolling out a new initiative – along with the associated additional paperwork – has been challenging at times. The introduction of a new product formulary to bring ESNEFT in line with the ACA and RCN’s (2021) guidelines, along with what was already happening in the community and our neighbouring trusts, led to most resistance, so work was needed to change the perceptions of staff. However, real improvements are beginning to show and an increasing number of colleagues now appreciate the importance of good continence care, assessing the patient and then selecting the most appropriate product to meet their continence needs. This was shown in the initial audit and anecdotal evidence received from staff, as well as patients, who told me they appreciated the opportunity to improve their continence.
Once staff were aware of good continence care, a number of them went on to ask for more training in this area. Staff on the pilot wards also told me they appreciated the additional support they were given to improve the care they could provide for their patients.
A continence policy is now being jointly developed with our community colleagues to provide consistent guidance for all of our staff. In addition, regular audits are being put in place across the trust to monitor this work and ensure it continues to benefit the quality of care our patients receive. These will be carried out by the continence nurse with the support of continence link nurses on the wards, which we are currently developing.
“Going forward, my future goal will be to inspire a positive attitude among all of our staff so we can provide good continence care for every patient”
Reflections
Although some wards have adopted the new continence assessment and care plan quickly and effectively, and are providing much-improved continence care as a result, support and training are still taking place in other areas where progress has been slower. The slower uptake became apparent during visits to the wards, which showed that some are more resistant to change, largely because staff felt the processes in place before the project began were sufficient to meet patients’ needs.
Making sure that education is available in a wide variety of formats has been a key element of the project and an important tool in helping us reach as many staff as possible. This has included lectures, small group teaching, e-learning and sessions held via Microsoft Teams – all of which have been led by the continence nurse, with support from the education department.
We are developing plans to train continence link nurses, who will then go back to their wards and share this learning with colleagues who, in turn, can encourage patients to try conservative treatment to improve their continence. As ESNEFT is such a large trust, this will be essential to the ongoing success of the service.
In the future, I plan to carry out another QI project, looking at the impact that introducing the continence assessment has had on patient care, including whether it has improved their overall continence and resulted in a reduction in falls and moisture-associated skin damage.
Conclusion
This initiative has shown that good continence care for hospital patients can be achieved and, in turn, reduce deconditioning, falls and moisture damage to skin, while also helping patients to regain their continence before they are referred to the community. Going forward, my future goal will be to inspire a positive attitude among all of our staff so we can provide good continence care for every patient admitted to East Suffolk and North Essex NHS Foundation Trust.
Key points
- Evidence suggests that continence care is often a low priority in acute trusts, with little training provided
- Poor continence care can have a major impact on quality of life, including leading to deconditioning and a loss of independence
- Patient safety is compromised as a result of poor continence care and can contribute to incontinence-associated dermatitis, falls and increased length of hospital stay
- Using the right assessments and products not only improves care and the patient experience, but also leads to cost savings for the NHS
Association for Continence Advice (2021) Understanding Continence Promotion. futurelearn.com (accessed 31 August 2022).
Association for Continence Advice and Royal College of Nursing (2021) Guidance for the Provision of Absorbent Pads for Adult Incontinence: A Consensus Document. ACA, RCN.
Featherstone K et al (2022) Understanding how to Facilitate Continence for People with Dementia in Acute Hospital Settings: Raising Awareness and Improving Care – An Ethnographic Study. University of West London.
Flanagan M (2020) Incontinence-associated dermatitis 2: assessment, diagnosis and management. Nursing Times; 116: 4, 40-44.
Moon S et al (2021) The impact of urinary incontinence on falls: a systematic review and meta-analysis. PLoS One; 16: 5, e0251711.
National Institute for Health and Care Excellence (2019) Urinary Incontinence and Pelvic Organ Prolapse in Women: Management. NICE.
NHS England (2018) Excellence in Continence Care: Practical Guidance for Commissioners and Leaders in Health and Social Care. NHS England.
Percival J et al (2021) ‘We tend to get pad happy’: a qualitative study of health practitioners’ perspectives on the quality of continence care for older people in hospital. BMJ Open Quality; 10: e001380.
United Kingdom Continence Society (2015) Minimum Standards for Continence Care in the United Kingdom: Report of the Continence Care Steering Group 2014. UKCS.
Voegeli D (2017) New insights on incontinence-associated dermatitis. independentnurse.co.uk, 2 June (accessed 28 February 2023).
Help Nursing Times improve
Help us better understand how you use our clinical articles, what you think about them and how you would improve them. Please complete our short survey.
Don't miss more great clinical content from Nursing Times
NT Bitesize learning videos – helping you to organise learning to fit in with your schedule
Clinical zones – keep up to date with articles in your clinical subject or nursing role/setting
CPD zone – user-friendly online learning units on fundamental aspects of nursing
Journal Club – clinical articles with discussion handouts for participatory CPD
Practical Procedures – 'how to' guides and teaching materials for clinical procedures
Self-assessment – clinical articles with linked online assessments for bitesize CPD
Systems of Life – applied anatomy and physiology to support your practice
 Nursing Times Resources for the nursing profession
Nursing Times Resources for the nursing profession 

Have your say
or a new account to join the discussion.