The human brain is the body's most protected organ, and for good reason.
To keep our body's 'control center' safe from pathogens and toxins, the brain and spinal cord sit in privileged exclusion from the rest of the body.
But this ivory tower also poses a significant barrier to medicine.
Today, virtually all large molecule drugs and more than 98 percent of small molecule drugs in the human bloodstream are unable to enter the central nervous system because of a 'locked gate' known as the blood-brain barrier.
Scientists say they are now closer than ever to smuggling important treatments through.
Researchers at the University of Pennsylvania have put together a simple model of the blood-brain barrier in the lab, allowing them to test the best drug transporters.
Specifically, the team is studying the delivery of fat-soluble 'packages', called lipid nanoparticles, which can pass through the blood-brain barrier and carry proteins, antibodies, or even messenger RNA with them.
This lipid packaging is what allows the mRNA vaccine for COVID-19 to enter the body's cells as well.
mRNA therapies hold great potential in treating neurological disease, as they can theoretically be used to replace missing proteins or edit faulty genes in the brain. But first, we have to get them there.
"Our model performed better at crossing the blood-brain barrier than others and helped us identify organ-specific particles that we later validated in future models," explains bioengineer Michael Mitchell.
"It's an exciting proof of concept that will no doubt inform novel approaches to treating conditions like traumatic brain injury, stroke, and Alzheimer's."
Such treatments are desperately needed. Excluding medicines that treat affective disorders, like antidepressants, some estimates suggest as few as one percent of all available drugs are active in the central nervous system.
To get around the blood-brain barrier, some drugs are directly injected into the brain, but this procedure is highly invasive, and the medicine does not diffuse easily throughout the organ, limiting its treatment scope.
In 2015, scientists used sound waves to allow chemotherapy drugs past the blood-brain barrier for the first time, spurring ongoing clinical trials. But this newest study takes a different approach.
Scientists have been studying lipid nanoparticles and their ability to deliver drugs to the brain for years now, but previous models could not measure how much mRNA actually made it to the central nervous system.
"I spent months figuring out the optimal conditions for this new in vitro system, including which cell growth conditions and fluorescent reporters to use," explains bioengineer Emily Han.
"Once robust, we screened our library of lipid nanoparticles and tested them on animal models."
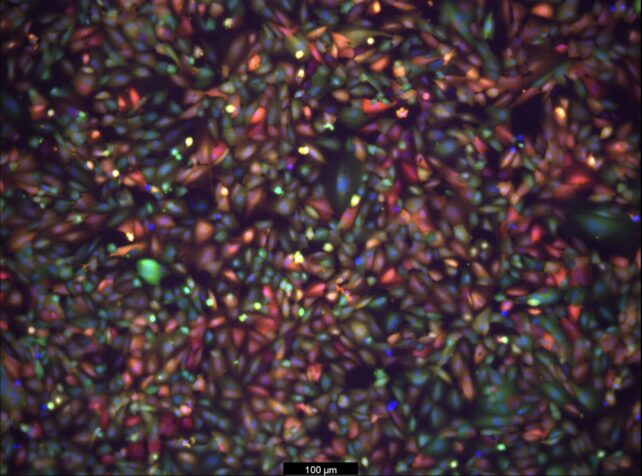
Of the 14 lipid nanoparticles the team tested in laboratory dishes, five were selected for further analysis in living mice.
These drug 'packages' – labeled with fluorescent markers – showed high transport across the blood-brain barrier.
When injected into the bloodstream of mice, some of the medicine generated a bioluminescent signal in brain cells that could be read by scientists as soon as six hours later.
Still, while some lipid nanoparticles managed to get across the blood-brain barrier, not all the medicine actually made it into brain cells.
This suggests that researchers need to be picky about which drug carriers they choose for future research.
The authors hope their new in vitro model will help scientists identify the top candidates, guiding the future development of brain-targeted treatments.
"Furthermore," the team at UPenn adds, "the platform could be re-engineered for studying lipid nanoparticle delivery to and across other biological barriers such as the blood-placental barrier, to study pregnancy-related diseases, and the blood-retinal barrier, to study retinal diseases."
The study was published in Nano Letters.