Scientists in Britain have revealed the role of a fertility “master gene” in one of the world’s first demonstrations of DNA editing in human embryos.
The study, which marks a first for the UK, could help uncover the cause of recurrent miscarriages and lead to more effective fertility treatments. It also raises ethical questions about the prospect of controversial gene editing techniques being used clinically to correct defects in, or even enhance, human embryos in the future.
Kathy Niakan, who led the work at the Francis Crick Institute in London, said: “Our research is the first time that genome editing has been used to understand the role of a gene in early embryonic development. This knowledge can be used to improve IVF treatment and improve our understanding of how some pregnancies fail.”
Niakan’s team is the first in Britain to have edited the DNA of human embryos, with just a handful of such experiments having been performed in China and the US. These focused on how editing might be used to prevent inherited diseases being passed from one generation to the next.
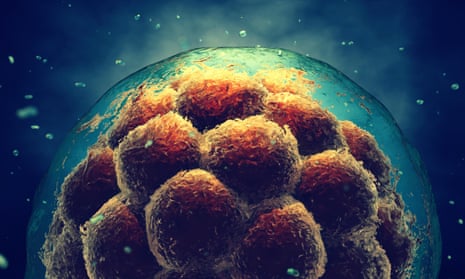
The latest work switches the spotlight to the basic biological sequence that plays out as a fertilised egg turns into a ball of cells, known as a blastocyst, during the first seven days of development. Only when an embryo successfully reaches the blastocyst stage does it stand any chance of implanting in the womb.
Quick GuideHow scientists discovered role of fertility 'master gene'
Show
What is Crispr?
Crispr, or to give it its full name, Crispr-Cas9, allows scientists to precisely target and edit pieces of the genome. Crispr is a guide molecule made of RNA, that allows a specific site of interest on the DNA double helix to be targeted. The RNA molecule is attached to Cas9, a bacterial enzyme that works as a pair of "molecular scissors" to cut the DNA at the exact point required. This allows scientists to cut, paste and delete single letters of genetic code.
Using 41 human embryos donated by couples with a surplus after IVF treatment, the scientists applied the gene-editing tool Crispr/Cas9 to make precise cuts in DNA and deactivate a gene called OCT4, which was believed to be important in the earliest stages of development. The study, published in Nature, showed this gene is critical for the embryo to make the transition from a uniform blob of cells to a blastocyst, which comprises three cell types that will go on to be the embryo, the placenta and the yolk sac.
Under a microscope, the edited embryos started by dividing and expanding normally, but then underwent repeated cycles of expansion and collapse without ever progressing to the next stage.
Scientists believe that lower than normal OCT4 activity could be why embryos fail to implant successfully, leading to miscarriage. Treating this would not necessarily require gene editing – it might be possible to coax more activity from the gene by changing the way embryos are cultured in the IVF process, for instance.
Kay Elder, study co-author from the Bourn Hall fertility clinic in Cambridge said that the technique could help improve IVF success rates, which remain frustratingly low. “Many embryos arrest in culture, or fail to continue developing after implantation,” she said. “This research will significantly help treatment for infertile couples, by helping us to identify the factors that are essential for ensuring that human embryos can develop into healthy babies.”
The failures of fertility treatments could be down, in part, to a reliance on mouse studies, which until now have been seen as the best way to work out the role of genes during embryonic development – and why things sometimes go wrong. The latest work highlights the shortcomings with this approach, showing that the OCT4 gene appears to play a different role in early human embryos than in mice.
“This is in a way unexpected, because of the dogma that the earliest stages of development are common for all mammalian and even some non-mammalian species,” said Dusko Ilic, reader in stem cell science at King’s College London. “The study is another proof that the findings from experimental animal models cannot be always extrapolated to humans.”
The latest work comes as an increasing number of researchers are applying the powerful genome editing procedure called Crispr-Cas9. The technique was invented only four years ago, but is already revolutionising biomedical research. It allows scientists to make precise edits to the genome – snipping through strands of DNA to deactivate genes and potentially correcting genetic flaws.
The technique could hold huge clinical potential, but it is also controversial because it involves altering the “germline”, meaning that any changes would be passed down to future generations.
Karen Yeung, professor of law at Kings College London, said: “The work demonstrates the invaluable role played by the Human Fertilisation and Embryology Authority in the British context in monitoring and ensuring that limits of responsible research on human embryos are respected, in order to maintain public trust in research of this kind.”