This is the eleventh in our job market paper series this year.
Malaria is preventable and treatable – but it is still deadly. In 2015, there were 214 million cases of malaria and an estimated 438,000 deaths. Nearly nine in ten cases occur in Sub-Saharan African, and the direct and indirect costs of this burden are high.
In my job market paper, coauthored with Josselin Thuilliez and Marie-Anne Valfort, we study the effects of contemporaneous, large-scale malaria control efforts in 27 countries in Sub-Saharan Africa. But we look at more than health – we focus on how malaria control brings about changes in household human capital investments.
Malaria control in Sub-Saharan Africa: Progress at last?
Previous efforts to curb malaria in Sub-Saharan Africa met with little success. In the 1950-60s, programs were characterized by “widespread disappointment and failure.” In the 1980-90s, they “fell into disrepair or were abandoned entirely.” Drug and insecticide resistance, as well as limited domestic health capacities, further hampered malaria control efforts.
Fortunately, the future of malaria control now looks brighter: Since 2000, cases are down by 42%, with death rates dropping by 66%. What changed? In 1998, the World Health Organization launched a new campaign to halve malaria deaths worldwide by 2010. This led to the creation of the Roll Back Malaria (RBM) Partnership, intended to harmonize the resources and activities among the many national, bilateral, and multilateral actors working toward malaria control.
But this turnaround comes at a price. By 2010, funding from external sources totaled nearly $2 billion per year. Policy-makers must evaluate if the results are worth the cost. And, in doing so, it is important to take a wide view – in other words, if these efforts are successful, do their effects go beyond health?
Big programs, big consequences
There is reason to suspect that large-scale efforts to reduce disease produce important economic outcomes (e.g., Jayachandran and Lleras-Muney, 2009). Case studies on historic eradication shape much of our understanding about malaria’s wide-reaching influence. Reducing malaria in early childhood can raise income and consumption, increase fertility, and improve educational attainment, literacy and cognition ( Bleakley, 2010; Cutler et al., 2010; Lucas, 2010; Venkataramani, 2012; Lucas, 2013; Barofsky, Anekwe and Chase, 2015).
This is because improvements in early childhood health can alter household decision-making. We show in a simple theoretical framework how these improvements serve as a catalyst to change household human capital investments. If, for example, the returns to education improve with better health, households may reduce their fertility and increase labor market participation in order to send their children to school. Using RBM, we can test for these relationships empirically.
Identifying Roll Back Malaria’s effects
We use the implementation of RBM to identify the effects of malaria control campaigns on human capital outcomes covering millions of individuals in 27 countries.
Compared to previous studies, we are able to tackle a large sample by combining data from several sources: geocoded household data from the Demographic and Health Surveys (DHS), detailed maps of malaria risk generated by the Malaria Atlas Project, and country-year disbursements from RBM’s earliest and largest funders. (RBM was driven, at the outset, by the Global Fund to Fight AIDS, Tuberculosis and Malaria, the President’s Malaria Initiative, and the World Bank’s Booster Program for Malaria Control in Africa.)
We develop a modified difference-in-differences (DD) analysis. Whereas a traditional DD would compute the treatment effect as the interaction between a respondent’s treatment status and an indicator for the post-treatment period, we proceed differently: We interact a respondent’s probability of belonging to the treated group (continuous from 0 to 1) with his or her continuous exposure to RBM campaigns.
RBM does not report sub-national data. However, because RBM targeted areas with higher initial malaria risk, a feature determined largely by geographic and climactic characteristics, we use an area’s pre-RBM malaria risk to proxy for its probability of treatment. More precisely, we use the Plasmodium falciparum parasite rate (PfPR) computed at the level of the DHS cluster. (See Bhatt et al., 2015 for further details.)
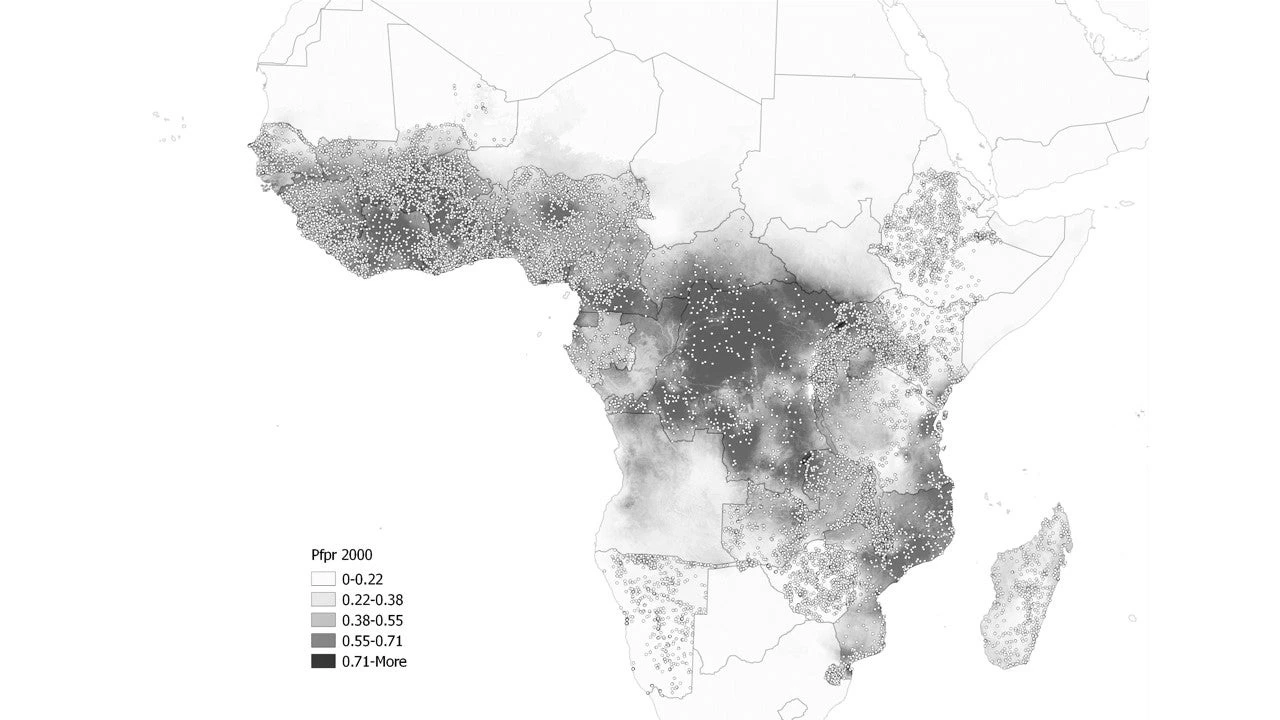
Figure: Spatial distribution of DHS clusters and initial malaria risk (Plasmodium falciparum parasite rate)
But we are still missing something: RBM scale-up occurred at different times in different countries. Respondents with the same probability of treatment could receive different levels of treatment depending on when RBM began, when they were surveyed, and their age at the time of survey. While we do not observe the same respondent in multiple surveys, we do observe similar individuals—those in the same age cohort—across time. Rather than using self-reported data (like bednet use), we proxy for exposure to treatment with the yearly amount per capita disbursed by RBM campaigns during a respondent’s lifetime.
The key point of this strategy is that it makes use of several layers of variation in exposure: cohort dates of birth, distribution of Demographic and Health Surveys across time, and RBM campaign start dates. Introducing differential treatment intensity within clusters has another, more practical, advantage: it allows us to control for cluster fixed effects as well as country-by-cohort-by-survey year fixed effects. In other words, the corresponding change in a respondent’s human capital outcomes is driven by variation in assignment to treatment at the DHS cluster level and variation in intensity of treatment at the country-cohort-survey year level.
Malaria control improves human capital
RBM successfully reduces mortality in an infant’s first year of life. But that’s not all: births decline, the probability of adult employment increases (as does the probability of wage work), and educational attainment grows. In our sample, for each additional dollar per capita per year at a constant level of malaria risk, the probability of infant mortality drops by 6.3 percentage points and children’s educational attainment increases by 0.4 years.
These results are consistent with similar studies. We provide evidence in support of parallel trends and run checks that address competing public sector expenditures, alternative treatment probabilities, sub-samples and other restrictions.
Implications for policy?
Mass interventions can help to break intergenerational health-based poverty traps and induce demographic transitions. Health is a key piece of this puzzle, especially for programs attempting to reduce but not eliminate health challenges. Conversations continue about how best to allocate future funds and how to improve value for money. Our results are especially meaningful in a landscape where health policies are shifting from vertical interventions like RBM to horizontal programs aimed at improving entire health systems.
Our time period could be considered at most medium-run, and the long-term effects of these programs certainly remain to be seen. The secondary effects of health interventions may never be large enough to compete with the intended health benefits. But our results show how improving health outcomes may have significant economic returns.
Maria Kuecken is a PhD candidate at the Paris School of Economics and Université Paris 1 Panthéon Sorbonne.
Malaria is preventable and treatable – but it is still deadly. In 2015, there were 214 million cases of malaria and an estimated 438,000 deaths. Nearly nine in ten cases occur in Sub-Saharan African, and the direct and indirect costs of this burden are high.
In my job market paper, coauthored with Josselin Thuilliez and Marie-Anne Valfort, we study the effects of contemporaneous, large-scale malaria control efforts in 27 countries in Sub-Saharan Africa. But we look at more than health – we focus on how malaria control brings about changes in household human capital investments.
Malaria control in Sub-Saharan Africa: Progress at last?
Previous efforts to curb malaria in Sub-Saharan Africa met with little success. In the 1950-60s, programs were characterized by “widespread disappointment and failure.” In the 1980-90s, they “fell into disrepair or were abandoned entirely.” Drug and insecticide resistance, as well as limited domestic health capacities, further hampered malaria control efforts.
Fortunately, the future of malaria control now looks brighter: Since 2000, cases are down by 42%, with death rates dropping by 66%. What changed? In 1998, the World Health Organization launched a new campaign to halve malaria deaths worldwide by 2010. This led to the creation of the Roll Back Malaria (RBM) Partnership, intended to harmonize the resources and activities among the many national, bilateral, and multilateral actors working toward malaria control.
But this turnaround comes at a price. By 2010, funding from external sources totaled nearly $2 billion per year. Policy-makers must evaluate if the results are worth the cost. And, in doing so, it is important to take a wide view – in other words, if these efforts are successful, do their effects go beyond health?
Big programs, big consequences
There is reason to suspect that large-scale efforts to reduce disease produce important economic outcomes (e.g., Jayachandran and Lleras-Muney, 2009). Case studies on historic eradication shape much of our understanding about malaria’s wide-reaching influence. Reducing malaria in early childhood can raise income and consumption, increase fertility, and improve educational attainment, literacy and cognition ( Bleakley, 2010; Cutler et al., 2010; Lucas, 2010; Venkataramani, 2012; Lucas, 2013; Barofsky, Anekwe and Chase, 2015).
This is because improvements in early childhood health can alter household decision-making. We show in a simple theoretical framework how these improvements serve as a catalyst to change household human capital investments. If, for example, the returns to education improve with better health, households may reduce their fertility and increase labor market participation in order to send their children to school. Using RBM, we can test for these relationships empirically.
Identifying Roll Back Malaria’s effects
We use the implementation of RBM to identify the effects of malaria control campaigns on human capital outcomes covering millions of individuals in 27 countries.
Compared to previous studies, we are able to tackle a large sample by combining data from several sources: geocoded household data from the Demographic and Health Surveys (DHS), detailed maps of malaria risk generated by the Malaria Atlas Project, and country-year disbursements from RBM’s earliest and largest funders. (RBM was driven, at the outset, by the Global Fund to Fight AIDS, Tuberculosis and Malaria, the President’s Malaria Initiative, and the World Bank’s Booster Program for Malaria Control in Africa.)
We develop a modified difference-in-differences (DD) analysis. Whereas a traditional DD would compute the treatment effect as the interaction between a respondent’s treatment status and an indicator for the post-treatment period, we proceed differently: We interact a respondent’s probability of belonging to the treated group (continuous from 0 to 1) with his or her continuous exposure to RBM campaigns.
RBM does not report sub-national data. However, because RBM targeted areas with higher initial malaria risk, a feature determined largely by geographic and climactic characteristics, we use an area’s pre-RBM malaria risk to proxy for its probability of treatment. More precisely, we use the Plasmodium falciparum parasite rate (PfPR) computed at the level of the DHS cluster. (See Bhatt et al., 2015 for further details.)
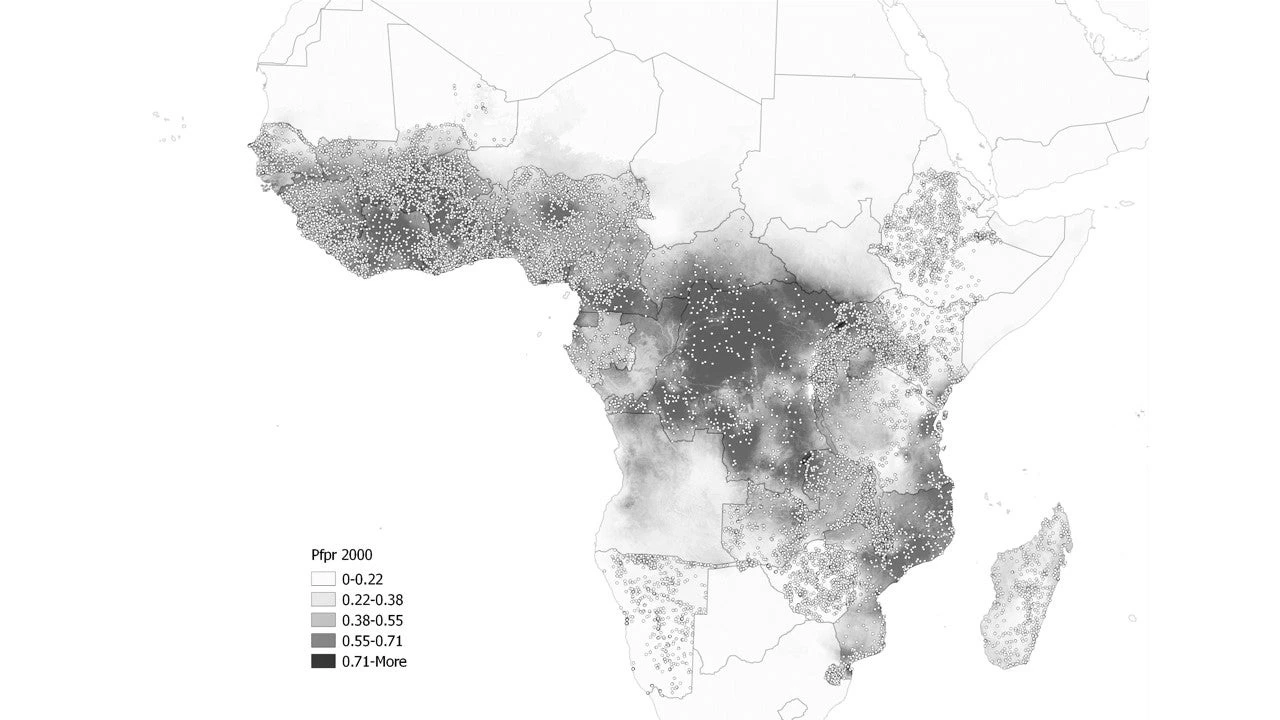
Figure: Spatial distribution of DHS clusters and initial malaria risk (Plasmodium falciparum parasite rate)
But we are still missing something: RBM scale-up occurred at different times in different countries. Respondents with the same probability of treatment could receive different levels of treatment depending on when RBM began, when they were surveyed, and their age at the time of survey. While we do not observe the same respondent in multiple surveys, we do observe similar individuals—those in the same age cohort—across time. Rather than using self-reported data (like bednet use), we proxy for exposure to treatment with the yearly amount per capita disbursed by RBM campaigns during a respondent’s lifetime.
The key point of this strategy is that it makes use of several layers of variation in exposure: cohort dates of birth, distribution of Demographic and Health Surveys across time, and RBM campaign start dates. Introducing differential treatment intensity within clusters has another, more practical, advantage: it allows us to control for cluster fixed effects as well as country-by-cohort-by-survey year fixed effects. In other words, the corresponding change in a respondent’s human capital outcomes is driven by variation in assignment to treatment at the DHS cluster level and variation in intensity of treatment at the country-cohort-survey year level.
Malaria control improves human capital
RBM successfully reduces mortality in an infant’s first year of life. But that’s not all: births decline, the probability of adult employment increases (as does the probability of wage work), and educational attainment grows. In our sample, for each additional dollar per capita per year at a constant level of malaria risk, the probability of infant mortality drops by 6.3 percentage points and children’s educational attainment increases by 0.4 years.
These results are consistent with similar studies. We provide evidence in support of parallel trends and run checks that address competing public sector expenditures, alternative treatment probabilities, sub-samples and other restrictions.
Implications for policy?
Mass interventions can help to break intergenerational health-based poverty traps and induce demographic transitions. Health is a key piece of this puzzle, especially for programs attempting to reduce but not eliminate health challenges. Conversations continue about how best to allocate future funds and how to improve value for money. Our results are especially meaningful in a landscape where health policies are shifting from vertical interventions like RBM to horizontal programs aimed at improving entire health systems.
Our time period could be considered at most medium-run, and the long-term effects of these programs certainly remain to be seen. The secondary effects of health interventions may never be large enough to compete with the intended health benefits. But our results show how improving health outcomes may have significant economic returns.
Maria Kuecken is a PhD candidate at the Paris School of Economics and Université Paris 1 Panthéon Sorbonne.

Join the Conversation